The treatment of a Grade 4 pressure ulcer with Algivon & Eclypse Adherent Sacral
Written by Sharon Dawn Bateman - RGN Di, BSc Hons, Ma - Clinical Matron - James Cook University Hospital, Middlesborough
Introduction
Miss B is an elderly lady aged 82 whose quality of life had been increasingly debilitated over the past eighteen months by a chronic deteriorating grade four sacral pressure ulcer.
Care at home had been compromised by a reduced immobility and left sided weakness resulting from a stroke, frequent urinary urgency often resulted in incontinent episodes and type 2 diabetes. These external conditions resulted in the development of a sacral pressure ulcer, sacral moisture lesions and reduced healing capacity generally. Miss B often felt depressed, isolated and lonely due to these conditions.
Miss B "I never thought that I would get a pressure sore, it's a terrible affliction."
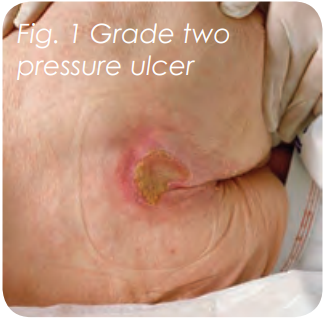
Miss B first developed a grade two pressure ulcer to her sacrum in 2009 following an episode of bed rest whilst recovering from a sever chest infection. Despite early intervention from the community healthcare tea and family members in regards to:
- Regular repositioning
- Air wave mattress
- Seat cushion
- A stable diabetes & high protein diet
- Strict hygiene regimen to maximise skin integrity
A plethora of wound care dressings and therapies had been implemented with little improvement, consequently the pressure ulcer continued to deteriorate eventually reaching a grade four status, this resulted in Miss B experiencing chronic referred pain to her mid flank region, burning sensations from the moisture lesion associated with her urinary incontinence, nausea from the analgesia regime and extreme social embarrassment resulting from the lingering malodour. She was often frustrated by the frequent changes within her dressing regime.
Miss B lived alone in a one level warden controlled facility with an extensive family network that provide daily support in ensuring that she maintained as normal a quality of life as is practically feasible. However, the chronic nature of the pressure ulcer and associated symptoms resulted in Miss B becoming socially isolated, withdrawn and unhappy.
Miss B: "I can't be bothered doing things I like anymore, I used to sire with my friends and knit but I can't do that anymore, not with this sore."
Assessment
Miss B was admitted to an acute elderly care ward. On initial assessment the wound bed appeared sloughy with a large central necrotic region and associated severe maceration around the wound margin radiating across both buttocks. The wound measured 8cm length x 10cm width x 5cm depth with a macerated 8cm peri skin border.
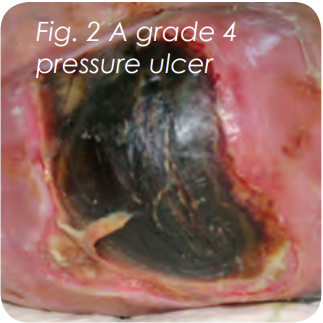
The ulcerative region did not demonstrate any visible areas of underlying healthy granular tissue and a strong malodour was present. Microbiology results indicated that the wound bed was indeed locally infected with the presence of Staphylococcus aureus, a common pathogen found in the infected chronic wound (White 2002).
The wound produced exudate of high viscosity and volume and the peri skin appeared fragile, macerated and inflamed. The patient's average pain score on dressing change was 8 out of 10 and 8 out of 10 on a continuous basis, this despite regular analgesia being administered.
The pressure ulcer had traditionally been managed using an application of a silver-impregnated antimicrobial, hydrofibre dressing, Aquacel Ag (Convatec), as the wound contact layer and a Tielle Plus (Systagenix), sacral dressing as the secondary dressing. Due to the associated problems of incontinence and secondary dressing creasing, Miss B required up to three dressing changes per day. The frequent dressing changes combined with the patient's moisture lesions further reduced her mobility and she had resigned herself to remaining in the same seated position until prompted to change it, a main concern was that she felt her movement encouraged the dressings to detach themselves putting extra strain on her nurses and family. This impacted on the patients ability to heal the pressure ulcer and may have directly linked to the deterioration from a grade two to grace four.
The European Pressure Ulcer Advisory Panel emphasise the importance of reducing static pressure and shear forces on any pressure point if skin damage is to be avoided or present tissue damage to deteriorate. The frequent removal of partially attached adhesive dressings resulted in inflamed peri skin and due to the unforeseen demand of the products the community team had to increase both nursing and pharmacy resources to meet the clinical needs, this occasionally resulted in the delay of dressing acquisition and delivery t the patients' home as a consequence heavily soiled dressings were being left in place. It was evident that implementation of a new dressing regime was advocated if wound healing was to be promoted. The option of utilising and advanced super absorbent sacral products (Eclypse Adherent Sacral - Advancis Medical) in conjunction with a Manuka embedded calcium alginate (Algivon - Advancis Medical) was discussed with both the patient and immediate family and consent as obtained.
Method
Algivon was applied and covered with an Eclypse Adherent Sacral secondary dressing twice a week for nine weeks.
The application of both products was simple, requiring nothing more than the Algivon being deployed at the wound bed and the Eclypse Adherent Sacral being placed over the wound and pressed into position.
Miss B: "The dressing change took no time at all and I did have to check it was all there when the nurse said she had finished... it felt like I didn't have a dressing on."
Results
At each weekly assessment and twice weekly dressing change the wound bed demonstrated a significant reduction in both circumference and depth. The necrosis and heavy malodour had resolved by week two, by week three there was a gradual reduction in slough and exudate production from heavy to medium, which resulted in a healthy granulating wound bed being made visible. The microbiology swab at week two demonstrated a clean wound with no evidence of increased bacterial bio burden and key to wound care management the patient pain score had reduced significantly to 2/10 on the numerical scale at the dressing change care intervention.
At week two the patient's mood and posture had improved significantly with Miss B changing her own position whilst seated independently and taking a more active role in her management regime and dietary intake.
Miss B: "I began to take an interest in what the nurses were saying and I wanted to help myself more like I used to before this sore began."
Weeks two and three highlighted a noticeable reduction in exudate production with the patient's wound being changed every third day in comparison to the thrice daily changes before the products being deployed and the 48 hour dressing changes at week one. By the forth week the dressing regime was reduced to every five days. This promoted more independence of the patient who could develop her own daily activity whilst on the ward without the disruption of wet, heavy soiled odorous dressings. Her pain score the following dressing change was a consistent 0/10 whilst the dressing was in place.
| Date | Length | Width | Depth | Clinical Status |
| 08.03.10 | 8cm | 9.8cm | 5cm | necrotic, sloughy, high exudate |
| 07.05.10 | 4.8cm | 4.8cm | 1.5cm | granular, epithelial with very low exudate |
Throughout the dressing regime utilising the Algivon and Eclypse Adherent Sacral therapies there was a noticeable reduction in overall wound size and depth, this had not been achieved within the previous eighteen months.
At the end of the nine week period Miss B passed away peacefully with her family at her side.
Discussion
Within today's healthcare climate patient's expect to receive the highest standard of wound care from experienced, knowledgeable caring clinicians who are familiar with advanced product which have a multi function in the streamlining of wound care dressing regimes, which reduce the impact and demand upon clinical resources and which are appealing to the patient.
Conclusion
The use of a product regime which incorporates both a medically impregnated calcium alginate, Algivon, in conjunction with Eclypse Adherent Sacral as a secondary dressing in the management of a chronic, deteriorating grade 4 sacral pressure ulcer has demonstrated a significant overall reduction in wound size and depth not previously achieved with various wound care regimes.
This case study dressing regime highlights the positive improvements of exudate management, pain reduction, odour control and non disruption of good skin integrity which are key elements within pressure ulcer healing processes. There has also been an important demonstrable improvement within the physical, psychological and social aspects of Miss B's healing wound care journey which resulted in a positive wound care experience for both the patient and the family members.
This was particularly valuable within this case study due to the terminal nature of the patient's medical status where the patient's quality of life, privacy and dignity and pain status were more of a priority than the actual end point of wound closure.
Family comments: "Our mum received the best overall care that we could have wished for... She passed away peacefully, in comfort and with her dignity in tact."
References
Bennett G, Dealey C, Posnett J (2004) The costs of pressure ulcers in the UK, Age and Ageing 33: 230 -35
Butcher M (2001) NICE Clinical Guidelines: Pressure Ulcer risk assessments and prevention – a review, World Wide Wounds, 1-3
DOH (1993) Pressure Sores: A key quality indicator, London DH
European Pressure Ulcer Advisory Panel (2009) Prevention and treatment of pressure ulcers: quick reference guide. Washington DC
Gray D, White R, Cooper P, Kingsley A (2004) The Wound Healing Continuum, An aid to clinical decision making and clinical audit, Wounds UK management supplement 9-12 London
Kirby P, Khan N, Dhillon N et al (2009) Do honey – impregnated dressings affect glycaemic control?, The Diabetic Foot Journal Vol 12 No 4 117-180
McCaffrey M (1983) Nursing the patient in pain. Harper and Row London
Mullai V & Menon T (2007) Bactericidal activity of different types of honey against clinical and environmental isolates of Pseudomonas aeruginosa, Journal of Alternative Complementary Medicine, 13:4, 439-441
Oryan A & Zaker S R (1998) Effects of topical application of honey on cutaneous wound healing in rabbits, Zentralb fur Veterinarmedicine A 45, 3, 181-8
White R, (2002) Trends in Wound Care, British Journal of Nursing Monograph Quay books Bath